Textbook of Polytrauma Management
Our comprehensive textbook provides a multidisciplinary approach to polytrauma management, covering all aspects of care from the injury site to rehabilitation. This essential resource brings together the expertise of leading international trauma specialists and offers evidence-based guidelines for the optimal management of severely injured patients. The textbook addresses critical topics including initial assessment, damage control surgery, ICU management, definitive treatment strategies, and long-term rehabilitation protocols.
This textbook serves as the foundational reference for our Polytrauma Course, providing participants with the knowledge base necessary for comprehensive trauma care. It features detailed protocols, case studies, and practical algorithms developed through decades of clinical experience and research.
View on Springer →Polytrauma Course Podcast Series
Join us for in-depth discussions on the latest developments in polytrauma management through our podcast series. Our episodes feature interviews with leading trauma surgeons, case presentations, and expert debates on controversial topics in trauma care.
Beyond the Broken Bone: Unpacking the Global Impact and Hidden Costs of Trauma
In this inaugural episode of the Polytrauma Academy Podcast, we delve deep into the far-reaching consequences of trauma beyond the immediate physical injuries. Our expert panel discusses the global epidemiology of trauma, the economic burden on healthcare systems, and the often-overlooked psychological and social impacts on patients and families.
Key topics covered: Hidden costs of long-term rehabilitation, socioeconomic factors influencing trauma outcomes, and innovative approaches to comprehensive trauma care.
The Golden Hour: Saving Lives Before the Hospital
In this critical episode, we explore the concept of the "golden hour" in trauma care - that crucial first hour after injury when immediate medical intervention can mean the difference between life and death. Our expert panel discusses pre-hospital care, rapid response protocols, and the vital role of first responders and emergency medical services.
Key topics covered: Optimal triage strategies, evolution of emergency medical services, communication between pre-hospital and hospital teams, and time-sensitive interventions.
Polytrauma's First Moments: Life-Saving Diagnostics and the "Treat First What Kills First" Imperative
This episode dives into the critical first moments of polytrauma care, focusing on rapid diagnostic decision-making and the fundamental principle of "treat first what kills first." Our expert panel discusses prioritization strategies in the trauma bay, essential diagnostic tools, and the systematic approach to identifying life-threatening injuries.
Key topics covered: ABCDE methodology in practice, point-of-care diagnostics, imaging priorities in unstable patients, and real-world case discussions.
Initial Assessment: The Foundation of Polytrauma Management
This essential episode covers the systematic approach to initial assessment in polytrauma patients. Our expert panel discusses the structured methodology for rapid yet comprehensive evaluation, ensuring no critical injuries are missed while prioritizing life-threatening conditions. Learn how experienced trauma teams conduct primary and secondary surveys efficiently.
Key topics covered: Primary survey protocols, secondary survey techniques, documentation and communication strategies, common pitfalls in initial assessment, and the role of team leadership in coordinating the evaluation process.
Coming Soon: Advanced Trauma Life Support in 2025
Join us for our next episode where we'll explore the evolution of Advanced Trauma Life Support protocols and discuss the latest evidence-based approaches to trauma resuscitation.
Coming Soon: Interdisciplinary Approaches to Polytrauma Care
Discover how different medical specialties collaborate in polytrauma cases, from the emergency department to rehabilitation, featuring interviews with leading experts from multiple disciplines.
Understanding Endotheliopathy in Trauma
Endotheliopathy refers to the dysfunction of the endothelium, the inner lining of blood vessels, which plays a crucial role in regulating blood flow, coagulation, and inflammation. In trauma patients, endotheliopathy can lead to increased vascular permeability, impaired coagulation, and dysregulated inflammatory responses. Recent research has highlighted the significance of endotheliopathy in the pathophysiology of trauma-induced coagulopathy and its association with adverse outcomes such as multiple organ failure and mortality.
Read Full Article →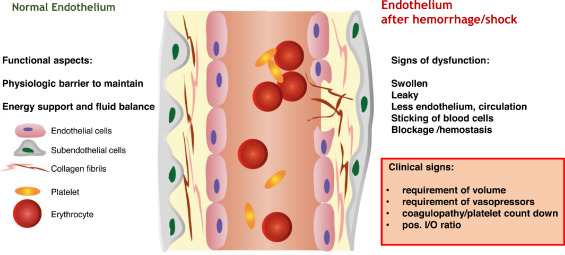
How High is the Surgical Load?
The study surveyed orthopedic trauma surgeons internationally to assess their perspectives on the surgical load in polytrauma patients and to quantify the impact of different fracture fixation procedures. Results revealed a consensus among participants regarding the importance of assessing surgical load, with a focus on intraoperative bleeding and soft tissue damage as significant factors. Surgeons prioritize staging procedures based on anatomical region, bleeding risk, and fracture complexity. Quantitative analysis showed variations in surgical load across different anatomical regions and types of procedures. Overall, the findings underscore the importance of individualized treatment planning and specialized training to optimize surgical decision-making in polytrauma cases.
Read Full Article →Surgical Treatment Strategy
There is still controversy surrounding the optimal strategy for definitive fracture fixation in polytrauma patients. The article outlines the historical dichotomy between "early total care" and "damage control surgery" approaches and highlights the need for a more nuanced, patient-centered approach that prioritizes safety. The review emphasizes the importance of repeated assessments in determining the appropriate timing and method of definitive surgery, considering factors such as patient physiology, clinical scenario, and injury severity.
Read Full Article →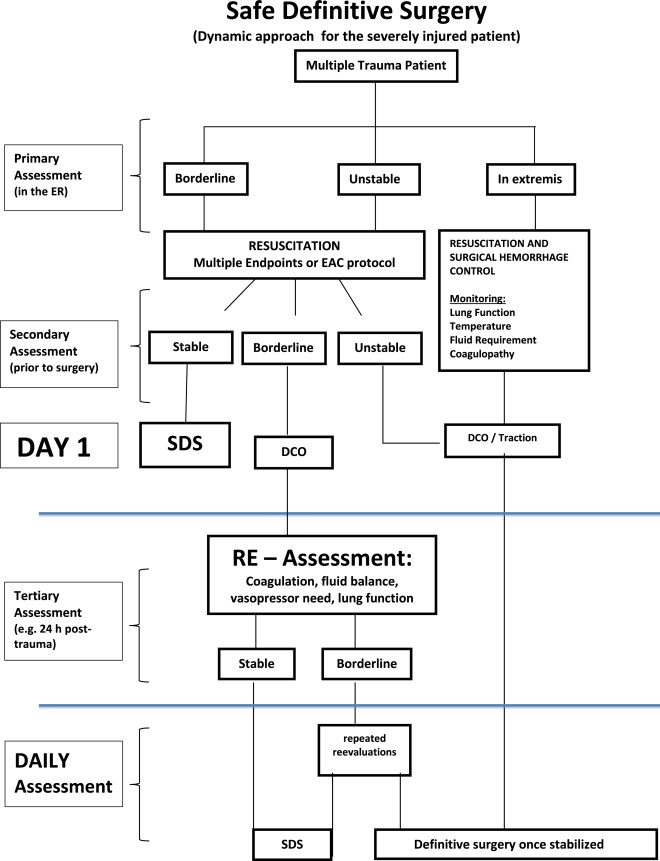
Which Treatment Strategy to Choose?
Does the injury distribution have an impact on surgical treatment strategies and outcomes in multiply injured patients with major fractures? The article addresses the ongoing debate regarding the timing of definitive surgery in such patients and aims to determine whether injury distribution correlates with specific surgical approaches.
Read Full Article →Why Do Polytrauma Patients Die?
The article examines changes in mortality patterns and causes of death among polytrauma patients over three decades. Through a review of literature from 1980 to 2008, it finds that while there have been no significant shifts in overall mortality patterns, deaths from hemorrhage have decreased in the last decade. Brain injury remains the primary cause of death, followed by exsanguination, sepsis, and multi-organ failure. The study suggests that advancements in trauma management, such as the implementation of the Advanced Trauma Life Support (ATLS) protocol and improvements in diagnostics and surgical techniques, have contributed to the observed reductions in hemorrhage-related deaths. However, further enhancements in early identification of brain injuries and ICU care are needed to address late mortality among polytrauma patients.
Read Full Article →Guideline for the Management of Major Bleeding and Coagulopathy
The guideline on managing major bleeding and coagulopathy in trauma patients underscores the global health challenge posed by severe trauma and emphasizes the need for local adaptation of guiding principles within institutions. Established by a pan-European, multidisciplinary task force, the guideline employs an evidence-based consensus approach, recommending direct patient transfer to trauma treatment centers and advocating for a restricted volume replacement strategy during initial resuscitation. However, challenges persist in identifying and managing patients pre-treated with anticoagulant agents. The guideline aims to standardize care across Europe and beyond, serving as an educational resource and basis for local implementation, with an emphasis on achieving measurable improvements in patient outcomes through multidisciplinary approaches and evidence-based practices.
Read Full Article →Which Parameters to Choose When Assessing the Pathophysiology of Polytrauma Patients?
The study evaluates four established scoring systems for their predictive abilities regarding early and late in-hospital complications in severely injured patients. Analyzing data from a level I trauma center, including 3668 patients, the study compares the clinical grading scale (CGS), modified CGS (mCGS), polytrauma grading score (PTGS), and early appropriate care protocol (EAC). Results indicate distinct differences in predicting complications, with PTGS showing the highest predictive value for late complications like sepsis and pneumonia, while EAC performs well in predicting early hemorrhage-induced mortality. The study suggests that incorporating values covering multiple physiological systems enhances predictive precision compared to systems focusing on single parameters, emphasizing the importance of comprehensive assessment in trauma patient management and score development.
Read Full Article →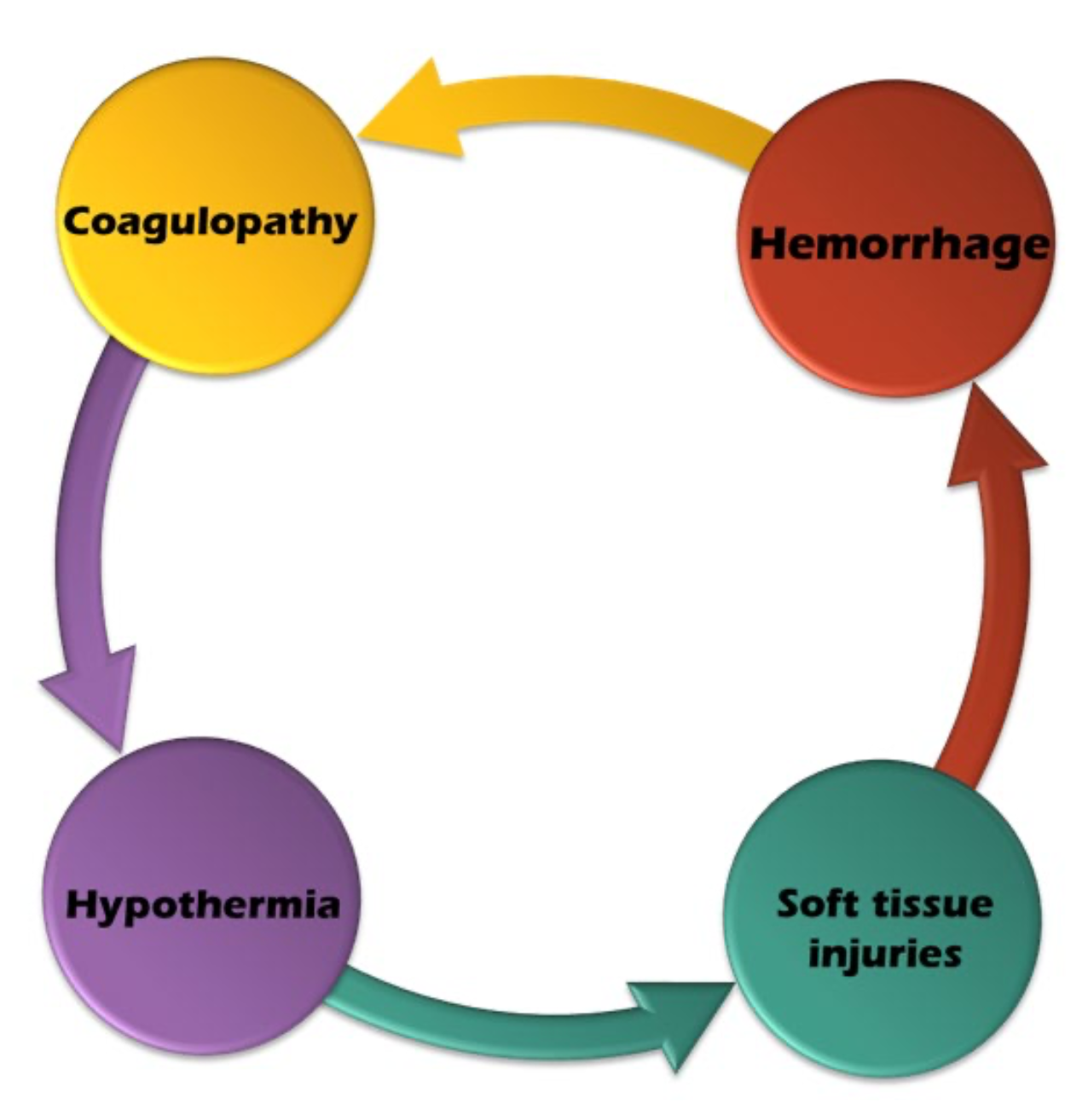
How Do Polytrauma Patients Do Further Down the Road?
The study assessed the health-related quality of life (HRQoL) of severely injured patients two years after trauma, focusing on pain, functional deficits, mental health, and socioeconomic impacts. Data from 129 patients treated at a trauma center between 2008 and 2010 were analyzed using the POLO-Chart questionnaire, European Quality of Life (EuroQoL), Short Form Health Survey-36 (SF-36), and Trauma Outcome Profile (TOP). Results showed that 62% of patients reported remaining pain, 64% had severe functional deficits, and 64% experienced decreased overall quality of life. SF-36 and TOP assessments confirmed impairments in various domains, including mental health issues like PTSD, depression, and anxiety. Socioeconomic consequences included hospital readmissions, long-term medication use, need for permanent care, inability to work, financial disadvantages, and job loss. The TOP instrument proved useful in identifying trauma-related impairments and guiding rehabilitation efforts. Overall, the study highlights the comprehensive impact of trauma on patients' lives beyond physical injuries, emphasizing the need for holistic rehabilitation approaches.
Read Full Article →Do Polytrauma Patients Suffer from PTSD, Anxiety or Depression?
The article investigates the long-term psychological effects of severe trauma on patients, revealing a significant incidence of psychiatric disorders such as PTSD, depression, and anxiety, which can impede the rehabilitation process. It highlights the importance of self-efficacy and family involvement in improving outcomes. The 20-year follow-up study, involving 337 patients, found that while the prevalence of full-blown PTSD was low at 3%, nearly half of the patients experienced symptoms related to PTSD, including intrusion, avoidance, or hyperarousal. Interestingly, the severity or distribution of injuries did not correlate with the development of psychiatric disorders, suggesting complex factors at play in long-term psychological outcomes. The study underscores the need for ongoing psychiatric support for trauma survivors, even decades after the initial injury, to address persistent mental health challenges and improve overall quality of life.
Read Full Article →The main results of the study indicate that more than half of polytrauma survivors exhibit symptoms of clinical depression or anxiety more than 20 years post-injury. Interestingly, injury severity was not found to be associated with the development of psychiatric sequelae, while non-injury-related factors such as prior psychiatric treatment and experiencing additional psychiatric insults after the injury were significantly linked to an increased risk of depression. These findings highlight the long-term psychological impact of polytrauma and emphasize the importance of identifying and addressing risk factors for psychiatric sequelae in this population to improve patient outcomes.
Read Full Article →